The room did not erupt with celebration. There were no raised voices, no dramatic gestures, no declarations of victory. Instead, there was silence — the kind that settles heavily, the kind that signals something serious has just been said.
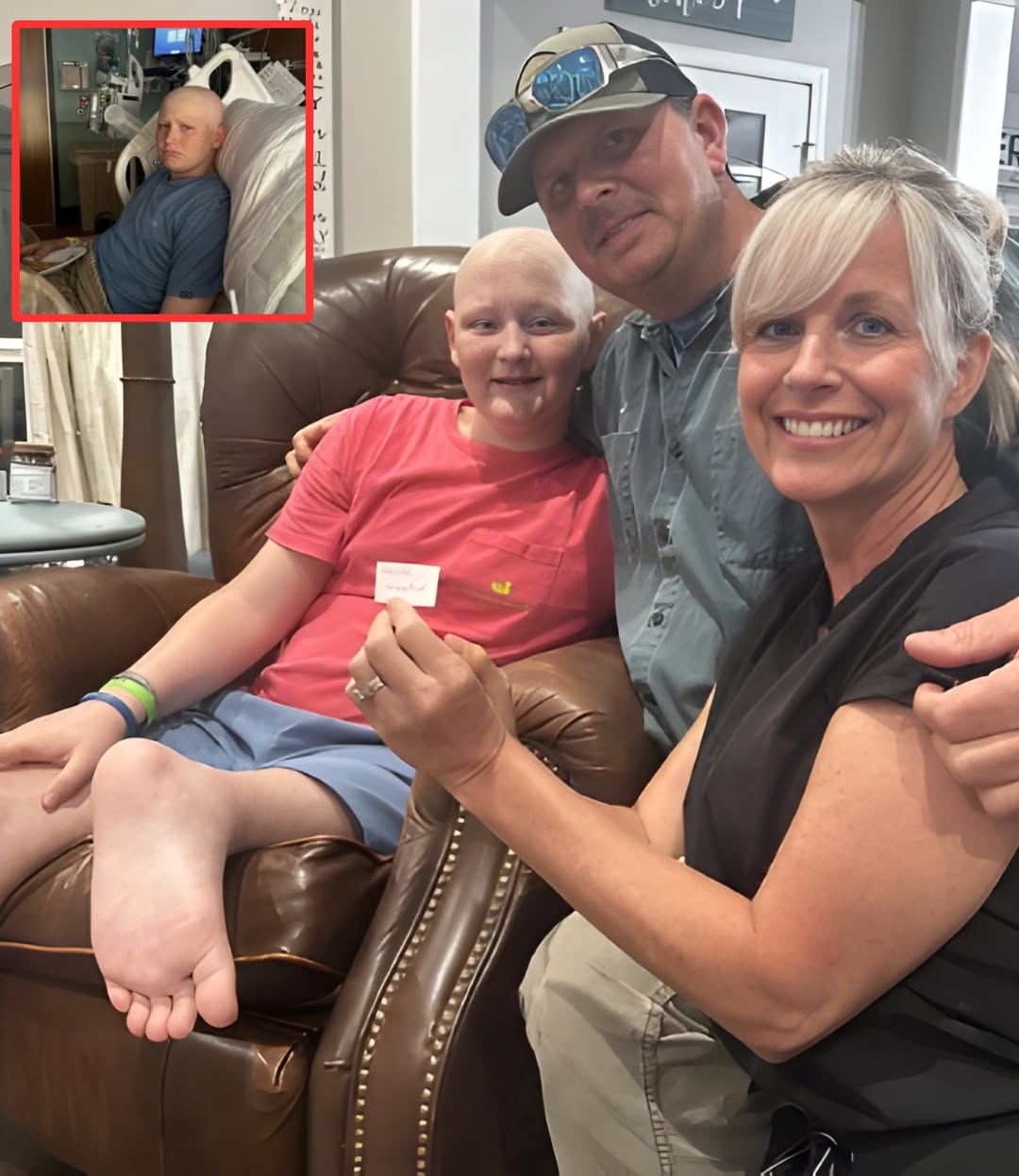
For days, that hospital room had carried exhaustion like a second atmosphere. Will Roberts, already worn down by a relentless battle with cancer, lay surrounded by the familiar rhythm of machines and muted conversations. His parents, Jason and Brittney, had reached a place many families know too well: the space where hope feels fragile, almost dangerous to touch. Treatments had taken their toll. New tumors had appeared. The future, once carefully planned in increments of scans and protocols, had begun to blur.
Then, quietly, everything shifted.
Doctors entered the room without fanfare. They did not frame what they were about to say as a breakthrough, nor did they soften it with optimism. Instead, they spoke carefully, deliberately, outlining a treatment plan that had not been on the table before. A different medication. A new method. A direct approach aimed specifically at the newly emerged tumors.
It was not described as a cure. It was described as a choice.
“This is a life-or-death gamble,” one physician said plainly, according to those present. Not reckless. Not rushed. But deeply calculated — considered only because the situation itself had reached a critical point.
For Will’s parents, the moment felt unreal. After days of despair that seemed to swallow every possibility of forward motion, they were suddenly being asked to consider a path that had not existed just hours earlier. The doctors explained the science behind it: how the medication works differently, how the delivery method targets the tumors more directly, how timing at this stage is everything. They also explained the risks — honestly, without cushioning.
This was not a miracle being offered. It was an option.
The decision came at one of the most sensitive stages of Will’s journey. His body has already endured more than most children face in a lifetime. Each treatment leaves a mark, not just physically but emotionally. The question was no longer simply about fighting harder, but about fighting smarter — and knowing when the two overlap.
As the doctors spoke, the room seemed to pause. Will listened quietly, his face unreadable, absorbing more than anyone might expect a child to. His parents exchanged glances that carried years’ worth of fear, faith, and exhaustion in a single look. They asked careful questions. They asked difficult ones. And they were given answers that did not promise safety — only intention.
Outside the room, life continued in ordinary ways. Nurses moved down the hall. Monitors beeped. Somewhere, another family laughed. But inside, time narrowed to a single moment of choice.
What makes this turning point remarkable is not just the medical shift, but the way it arrived. There was no dramatic escalation leading up to it. No sudden improvement. Instead, it emerged from persistence — from doctors unwilling to surrender to protocol alone, and from parents who refused to stop advocating, even when exhaustion made every conversation feel heavier than the last.
In oncology, especially pediatric oncology, moments like this are rare and weighty. Changing course mid-journey is not done lightly. Every adjustment carries consequences, and every decision must balance urgency with caution. To introduce a new medication and method at this stage signals both concern and commitment — concern about the disease’s progression, and commitment to doing everything possible within reason.
For Will, the coming days will not be easy. This new plan does not erase the pain he has already endured, nor does it guarantee relief. But it represents something essential: movement. In a fight where stagnation can be as dangerous as decline, movement matters.
His parents have spoken often about the emotional toll of waiting — waiting for scan results, waiting for pain to ease, waiting for answers that sometimes never fully arrive. This decision, however daunting, breaks that cycle. It replaces waiting with action.
There is also something deeply human in the way this moment unfolded. No cameras. No announcements. Just doctors and a family facing reality together. In a world accustomed to medical headlines framed as wins or losses, this story exists in the in-between — where courage looks like choosing an uncertain road because standing still is no longer an option.
As Will prepares to begin this new phase of treatment, the atmosphere around him has subtly changed. Not lighter, necessarily — but focused. Intentional. His care team is watching closely, adjusting carefully, aware that every response matters. His parents remain by his side, steady even when fear threatens to resurface.
This is not the end of Will’s story, nor is it the resolution many hope for. It is a chapter defined by quiet bravery — by a family saying yes to possibility, even when it comes wrapped in risk.
One detail from that conversation between doctors and parents continues to echo in their minds — a reminder of just how narrow the margins are, and why this decision could shape everything that follows. It is a detail they are not yet ready to share publicly, not because it lacks importance, but because it carries weight still being processed.
For now, what matters is this: in a moment when hope seemed dangerously close to fading, it did not disappear. It changed form. And sometimes, that is enough to keep moving forward.
Will’s journey continues — not with cheers, but with resolve.


Leave a Reply